bestfootdoc
Displaying items by tag: bestfootdoc
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Treatment Options for Arthritis of the Big Toe

Arthritis of the big toe or sometimes called hallux limitus or hallux rigidus involves degenerative arthritis of the big toe. It often presents as pain and swelling in the big toe and even limited range of motion. Patients often have a history of any injury like a turf toe type incision where the majority of the time this is genetic in origin. This typically starts from an anatomical misalignment or elevated first metatarsal where long-term jamming of the joint and pain and swelling begins.
The treatment options from a surgical aspect involves joint preserving procedures. Joint sparing procedures involve trying to increase the life of the joint.
Joint sparing procedures typically have consisted of cleaning up the joint which is very commonly called a cheilectomy. This can be done for early type arthritis. This has all been considered were course of early intervention and has had great outcomes.
Joint destructive procedures typically involve the use of implants or fusion. Implants of the big toe joint have fallen out of favor and are not utilized by many physicians. The stays and fusion continues to be the mainstay. However there are other options that become available, depending on the patient's needs. There are some physicians that advocate what is called an interpositional arthroplasty which seems to work well and provides some space in the joint to provide cushioning.
If you have big toe pain I am happy to help make an appointment at our office and we can see whether conservative or surgical options are warranted. Give us a call today at 425-391-8666 or make an appointment online today.
Sincerely,
Brandon Nelson
Board-Certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Minimally Invasive Bunion Surgery

Bunion surgery has progressed significantly since its inception. Years ago, it was not uncommon for patients to stay overnight in the hospital if they had bunion surgery. Often times patients would spend days in the hospital and be in a cast and nonweightbearing for months. However this is a very rare occurrence these days and the majority of procedures are performed in an outpatient setting and very rarely is there an extended period of nonweightbearing. This evolution of bunion surgery has allowed for minimally invasive surgeries to become more commonplace.
Minimally invasive refers to making significantly smaller incisions than we’ll we typically do for bunion surgery. The average bunion can now be performed with minimally invasive surgery through an approximate 2 cm incision. The advantages of minimally invasive surgery is it allows for a quicker recovery and increased healing capacity. The majority of people will heal more quickly than the traditional open bunion procedure and will have less pain.
It is important to note that not every patient is a candidate for minimally invasive bunion surgery as it depends on other factors including overall foot structure and size of the bunion. It is important to have a thorough evaluation and workup for considering bunion surgery, any type of bunion surgery including minimally invasive. If you’re having bunion pain please contact my office and we will be able to get to an appointment and have your bunion evaluated. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Board-certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician, Talks About Ingrown Nails

Ingrown nails can be extremely uncomfortable. They are caused from a bacterial infection typically in the big toe. Often times patients will have a history of ingrown toenails or family history of ingrown toenails. It is important to not try and treat ingrown toenails at home as this typically will make the infection worse. Ingrown nails themselves typically present as pain and swelling along the border of the toenail where the skin, patients will experience some drainage from the site and is often painful at times.
I recommend patients are evaluated when their nails are sore, red, thickened or painful with walking. There are many different options for treating an ingrown nail however typically the offending nail border has to be removed. Once removal is performed the procedure of choice is really dictated by the number of ingrown toenails the patient has experienced. The two options are an incision and drainage or what is called a matrixectomy.
Option one or incision and drainage involves removal of the offending nail border. This is typically done on just the side that is painful. Prior to removal the toe is anesthetized, cleaned and sterile prep. Nail is then removed with the hemostat appendicitis, flushed and covered with a sterile compressive dressing. Typical recovery from something like this is patients can return to activities the next day or so once a day for 1 week.
A matrixectomy involves a similar technique as described above. However once the nail is removed the nail cells are cauterized to prevent them from growing back. Matrixectomy is a procedure specifically designed for someone that has a history of recurrent ingrown toenails or long family history of ingrown nails. The patient’s toe will be red and sore often times for 2-3 weeks after the procedure.
If you’re experiencing painful swollen digit please give me a call today and I can help 425-391-8666, or make an appointment online.
Sincerely,
Board-Certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Forefoot Capsulitis

Capsulitis refers to a large group of conditions that is associated with inflammation of the joint capsule. It is important to have a little bit background of anatomy in order to understand this pathology. The joint is where 2 bones come together and these 2 bones are covered with articular cartilage and then these 2 bones are encapsulated by the joint sac that is full of fluid or hyaluronic acid. These all work in tandem to provide functional smooth gliding joint. There are many causes of capsulitis, basically it is just inflammation of the joint capsule itself.
Dr Timothy Young, a Board Certified Foot Surgeon, Talks About Supartz (Synthetic Joint Lubricant)
Dr. Timothy Young has used this treatment for arthritis in the foot and ankle for over 10 years. This has been one the most effective nonsurgical options that we have. Supartz is synthetic joint lubricant Sodium Hyaluronate, and this is very joint and cartilage protective.
On the other hand, another common injection used by many clinics is cortisone. Cortisone can be very damaging to joints and cartilage especially with repetitive use. It can weaken the joint capsule and cartilage and over time accelerate the degenerative process. Supartz does not have these degenerative properties in fact quite the opposite, it is very protective.
Applications: Arthritis of the great toe joint is one the most common applications. But arthritis and joint pain from the ankle is another common treatment site along with other joints in the forefoot and midfoot. '
Duration: We have found that Supartz injections can provide relief and last between 6 and 12 months.
The local anesthetic is utilized initially so that there is no pain during the Supartz injection itself. Also during the Supartz injection Dr. Young utilizes ultrasound imaging to pinpoint the location and make certain that the Supartz goes directly into the joint as intended.
For a live video showing Dr. young doing a Supartz injection for great toe arthritis see youtube: https://www.youtube.com/watch?v=kZ9Rc6B8Fqc (Search: BestFootDoc Supartz YouTube)

If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses How Doctors Diagnose Resistant Plantar Fasciitis

One of the essential tools for evaluation of heel pain is ultrasound high definition imaging. With this diagnostic tool, we can see if the planter fascia is excessively thickened and to what extent. For example typical thickness would be 3- 4 mm. But in severe cases it can be 7 mm or even up to 11 mm thick. This can be especially helpful when comparing to baseline or the non-symptomatic side.
In some cases there has been plantar fasciitis in the past on the non-symptomatic side or some individuals have plantar fasciitis affect on the both the right and left foot which does make baseline comparison a challenge. So when we see a severe case of plantar fasciitis with severe thickening of the fascia then we know it will be even more resistant than typical. That means that we have to consider some some of the treatment options for resisting cases such as shockwave therapy or PRP. We still have to do all of the other traditional treatments for plantar fasciitis.
Give us a call at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board-Certified Physician and Surgeon, Discusses How to Get The Best Bunion Surgery

Bunion surgery can be overwhelming to think about, really any surgery can. In general, I see a few patients a day with questions about their bunions and about bunion surgery. I believe the process can be simplified when the surgeon you see has both experience and timelines to help you understand the entire process.
Most bunion surgeries can be done in an outpatient setting. At my office office, we are lucky enough to have an onsite surgery center which is both a huge cost and time savings. It also allows me to operate on more bunions and has provided me with a well of experience. It is important to understand that experience and the number of bunions a surgeon sees makes a dramatic difference.
Most bunion surgeons do two types of procedures one in the head of the 1st metatarsal and one in the base. The 1st metatarsal is the bone with the bunion deformity. The head procedures allow patients to walk right after surgery and is used for small to medium bunions. The base procedures usually require about 3-4 weeks of non-weight bearing. This procedure is usually for pediatrics or larger bunions. Both can provide excellent correction when used appropriately.
If you are thinking about bunion surgery come see me and I can be of some help with the process. Give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board Certified Surgeon Talks About Midfoot Arthritis.

As we all get older there will always be some degenerative arthritic changes. One of the more common type is degenerative joint disease. This primarily affects the weightbearing joints of the body including the foot. In addition to normal wear and tear, some individuals have a foot structure that is much more prone to increased and disproportionate stress loads through the midfoot. The stress loads are one of the biggest factors leading to long-term arthritis of the foot. For example, an individual that has a large bunion, will often have poor mechanics and weightbearing function of the first metatarsal-this bone is designed to bear up to half the weight of the whole foot especially through propulsion and push off during gait. When this does not happen, a disproportionate stress load goes through the next in line second metatarsal. Eventually that stress load can manifest at the base of the second metatarsal where it articulates with the second cuneiform.
Over time this increased and disproportionate stress load causes premature and excessive wearing through this joint. Initially there is dorsal compression on the joint causing bone spurs on the top of the joint and increased wear and tear on the articular surfaces with thinning of the articular cartilage. Eventually this can become bone-on-bone. In mild and moderate early cases this can be treated mechanically with orthotics and appropriate shoes. As it becomes more pronounced and more severe than additional treatment options can be considered. At the moderate stage often times sympathetic joint lubricant can be utilized. It is critical to use ultrasound imaging to make certain that this synthetic joint lubricant goes directly into the appropriate joint. Our clinic typically utilizes supartz brand sympathetic joint lubricant. This same highly viscous solution is used, only in the knee and that is where the initial studies for utilization were done. If it is primarily a problem with a painful bone spurs on top then these can be surgically removed. However, usually this is just the tip of the iceberg and in severe cases the second metatarsal–cuneiform joint should be surgically treated with a fusion. This stabilizes the joint and illuminates the damaged cartilage and excessive motion here.
Give us a call today at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician and Surgeon, Discusses the Best Long Term Treatment for Plantar Fasciitis
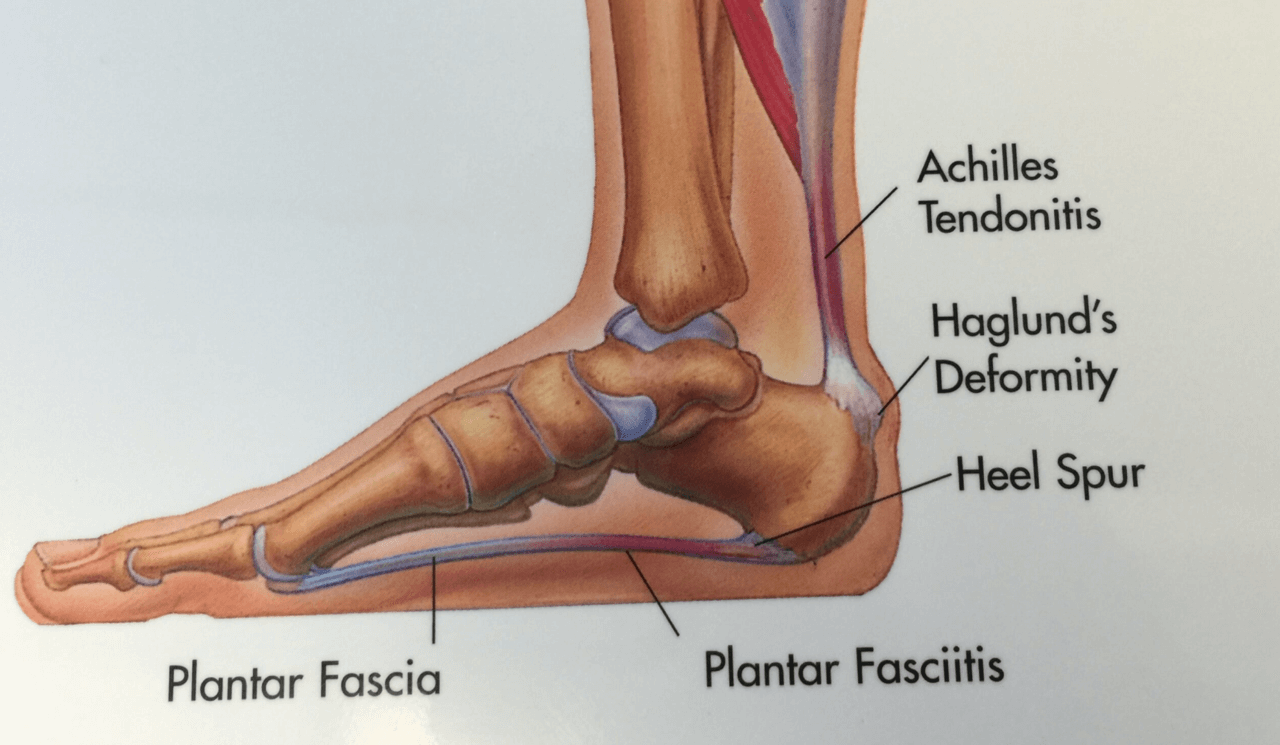
Plantar fasciitis continues to be the most common source of heel pain. The majority of our heel pain patients are still presenting with fasciitis. Patients usually feel pain in the morning or after sitting for a short period of time. The symptoms can range from burning and tingling in the heel to a bruised like sensation when walking. There does not need to be any history of trauma or even an increase in exercise. The major causes continue to be anatomical and foot structure related.
I can tell you I have been treating plantar fasciitis now for almost 15 years. I would say a conservative estimate is probably close to 10,000 patients that I have treated for heel pain. I have learned a lot with this time and quantity. I continue to read and learn and study each patient. This has provided me with a unique perspective. I would say I am probably one of the foremost experts on heel pain.
The best long-term treatment to date that I have discovered is utilizing one’s own biology to heel the plantar fasciitis. This condition is created when the fascia is overworked and needs to be strengthened structurally and functionally. The technique I utilize is unique to my practice and has taken years to perfect. Basically I harness a patient’s natural ability to heal and utilize that to repair the fascia. There is no down time, and the success rate is close to 97%. If you suffer from fasciitis make an appointment today and I will help.
Give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, a Board Certified Bunion Expert, Discusses Bunion Surgery and Covid-19

Bunion surgery and even surgery in general requires planning. Covid-19 has created a new work environment for a lot of people in Washington State. A larger percentage of people are working from home and have decided this provides an opportunity for them to have bunion surgery.
Surgery in general can be challenging, trying to find the correct time and date, planning for the recovery and taking time off work. However, we have seen quite a few people this year that have found working from home to be an advantage for surgery recovery. Without the need for a commute recovering at home and working has seem to work well.
I agree with these patients as foot and ankle surgery often requires modification to one’s work schedule. People working from home have a great opportunity to get the surgery they have been putting off. I think that this is a silver lining of Covid-19. I have personally seen our surgical load increase this year as people want to have elective surgeries they have been procrastinating.
I still think it is important to plan ahead. I like to provide my patients with all the information they require so they can prepare and make their recovery easier. Being preparde can make the surgical process much easier. Getting your house ready, making sure you have a way to get around, setting up a work station all these little tips make a big difference.
If you have a bunion or have been waiting to have surgery on your foot or ankle now is a great time. Give us a call today at 425-391-8666 or make an appointment online.
Google Business Reviews Error Notice!
Read Below Steps Carefully :
1. Check your API key and PLACE id. May be it is not right. Make sure it is correct one.
2. This message commonly shows when api key is exceeded daily request quota for this API or there is no active billing account for this API. Because according to Google there is a limit for free API key. If it exceeds they ask for billing.
3. To know more about Google Pricing , Check here : Google Pricing
4. You can create your Google API key here
5. Must use a right PlaceID. Get PlaceID here
6. One important thing, Don't forget to add billing account to Google. Must check what Google says here
7. If you still find issue , then check first if your Business registered with Google or not. Read more about it here
8.Still find issue, then contact developer : info@aaextensions.com or ashik685@gmail.com